Understand the disease what is osteoarthritis?
- Introduction
- What is osteoarthritis?
- What are joints?
- What is osteoarthritis?
- Is it common to osteoarthritis?
- Where can one suffering from arthrosis?
- Factors influencing the onset of osteoarthritis?
- Does symptoms lead to osteoarthritis?
- How is arthritis diagnosed?
- How is osteoarthritis treated?
INTRODUCTION
Arthritis is a very common disease in human beings. You've probably heard about of osteoarthritis and it is possible that your doctor has diagnosed the disease or know someone who suffers from arthritis.There is much confusion among the people about the concepts of "rheumatism" and osteoarthritis. Many people don't really know what are these terms. There are people who say that it has "rheumatism" when you have pain in your back or limbs. Many times patients believe that osteoarthritis and "rheumatism" are the same process and, on the other hand, sometimes have the idea that it's different diseases.
The truth is that the term "rheumatism" as such does not exist in medicine. Instead use the concept of rheumatic disease or rheumatism. Rheumatic diseases are actually a very broad group of diseases, different in terms of their cause, evolution and treatment. However, all of them have in common that affect any structure of the musculoskeletal system of the human body. So, say that someone has "rheumatism" is so vague and nonspecific as saying that you have "heart, lung or bowel", for example.
The musculoskeletal system is made up of bones, joints, muscles and tendons. Thanks to the musculoskeletal system we can move, move, and ultimately, all activities of our daily lives (walk, write, work, eat, exercise...). Rheumatology, therefore, is the specialty of medicine that treats all diseases of the bones, joints, muscles and tendons.
Of all the different rheumatic diseases, most importantly, by its frequency and impact on society, is osteoarthritis. There are other types of rheumatism, such as osteoporosis, arthritis, tendinitis, drop, etc., that people sometimes confused with osteoarthritis. The cause of this confusion is that can cause similar symptoms (pain, difficulty to move...). However, each of them has different a cause and treatment.
Following, are different aspects of arthritis that may be interesting to the reader. The aim is to present in a didactic and simple, understandable way for an audience of non-expert on medical topics, issues and ideas most relevant in relation to osteoarthritis.
WHAT IS OSTEOARTHRITIS?
We have already mentioned that the arthritis is a rheumatic disease. Osteoarthritis is a disease that affects the joints and is by far the pathology to articulate more frequent and important.Osteoarthritis is characterized by the progressive loss of the cartilage of the joint due to wear. This wear and tear of the cartilage is favored by the use of the joint and the passage of time. Furthermore, the deterioration of cartilage depends on other factors which, apart from age, contribute to hurt you.
Osteoarthritis is a chronic disease; that is, that it lasts a lifetime. However, and although you can make progress with the passage of time, with an appropriate treatment can be controlled. Therefore, you should not necessarily cause pain and disability in people who suffer from it.
WHAT ARE JOINTS?
The joints are the joints between the ends of bones, which allow some movement among them. This mode, extremities and back can bend, turn...In the joint, each end of the bone is covered by a hard tissue, although with certain elasticity and flexibility, which the cartilage is articular. Cartilage facilitate movement between the bones and act as a buffer between them, avoiding that they directly rub bone with bone. Cartilage is a tissue that is comparable to the "pizzle" found in some parts of animals that we consume as food.
To complete the gear, which is a joint, all this structure is shrouded in a bag called capsule articulate. Capsule joint is reinforced by ligaments, which are bands of tough fibrous tissue. Ligaments provide stability to the joint. They are responsible for prevent joints is luxen or "disloquen" when they are subjected to a forced movement.
Finally, bathing the inside of the joint, there is a small amount of liquid, which is called synovial fluid. Synovial fluid acts as a lubricant of all this machinery which is a joint, facilitating movements. This fluid is produced by a thin layer of tissue called synovial membrane. The synovial membrane is located, upholstering articular capsule inside, in areas in which there is no cartilage.
Schematic view of the structure of a normal joint.
WHY THERE ARTHRITIS?
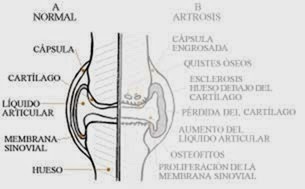
As mentioned, osteoarthritis is caused by degeneration and wear of the cartilage of the joint. In osteoarthritis, the cartilage loses consistency and elasticity, and its surface is cracking and progressively eroding. Cartilage erosion conditions to gradually decrease its thickness, and can even get to disappear completely with the passage of time. Protection function that has the cartilage is lost with its disappearance, and exposed ends of bones, touching each other "bone bone". According to cartilage loss is occurring, the bone that is located below is also affected and reacts. The injured bone responds to becoming more dense (in medicine is called bone sclerosis), emerging "cysts" inside the bone (called geodes). New bone that grows is also formed by the edges of the joint, as spikes or burrs of bone, which are called osteophytes.In addition, all of these lesions that occur in osteoarthritis, condition the synovial membrane is inflamed. When it ignites, the synovium becomes thicker and can produce more than the normal synovial fluid. Therefore, a joint with osteoarthritis is sometimes inflated to contain excess fluid (spill articulate).

Schematic view of the structure of a joint affected by osteoarthritis.
The loss of cartilage, the bone spurs and swelling of the joint make that, in osteoarthritis, we can observe externally how joint is deformed. In more advanced stages the bones lose times its normal alignment. Spine wear articulate, which characterizes osteoarthritis, it starts in structures that are referred to as intervertebral discs. The intervertebral discs are a kind of elastic pads with a central portion or nucleus of gelatinous consistency. The discs are located between vertebra and spinal vertebra. Its function is to dampen charges suffered by the column and allow the movements of the same. Thanks to this, all the vertebrae and their intervertebral discs altogether form a flexible structure.
When osteoarthritis in the spine, these intervertebral discs suffer a loss of their water content and its elasticity. In this way, disk progressively decreases its thickness. This decrease in disk height is what is called commonly "pinched disk". With progressive wear of the disc, gradually increases the contact and friction between the vertebrae, which also react to becoming denser (bone sclerosis) and forming bone burrs on the edges (the osteophytes).
Schematic view of the spine.
Changes that occur in osteoarthritis of the spine.
IS IT COMMON TO OSTEOARTHRITIS?
Arthritis is a very common disease. More than 80% of people 75 years and older are affected by this disease. In addition, it is possible to find some alteration of osteoarthritis in more than half of people older than 65.However, it is important to note that, although the doctor detected accidentally in some x-ray signs of arthrosis, joint less than half of the people that have changes of wear present symptoms.
Although arthritis is manifested most significantly in the elderly, this is not always true. For this reason, you should not be considered an alteration "own years" or exclusively due to the aging, but it must be taken into account as a real disease. Osteoarthritis is a disease of very slow progress. It starts many years before arriving at advanced ages of life, and it should be diagnosed and treated as soon as possible to improve their prognosis.
Osteoarthritis is a disease more common in women. Women are more likely to suffer from disease, especially in the joints of the hands and knees.
WHERE CAN ONE SUFFERING FROM ARTHROSIS?
Osteoarthritis can affect any joint of the upper limbs (arms, hands), lower limbs (legs, feet), as of the spinal column.However, osteoarthritis tends to occur mainly in those joints subjected to higher overhead movements or greater weight.
Extremities, osteoarthritis affects mainly the fingers of the hands, knees, hips and toe of the foot. In the spine, the neck (cervical spine) and low back (lumbar spine) are regions that commonly develop osteoarthritis.

Most frequent anatomical sites of osteoarthritis.
Arthritis that develops in other than those listed joints is much more uncommon. If it occurs, tends to be related with some trauma or old fracture, or some other type of injury or joint disease earlier, that have contributed to that joint wear. Arthritis may have a single joint (knee or hip arthritis...), or may affect many joints at the same time (what in medicine is called polyarthrosis). This circumstance is of importance in the face of the prognosis and treatment of the disease.WOULD WHAT FACTORS INFLUENCE THE ONSET OF OSTEOARTHRITIS?
There are several factors that have a direct relationship with the development of osteoarthritis. The most important are the following: obesitySuffering from overweight have a relationship well established with the development of osteoarthritis in the knees (the obese have more osteoarthritis of the knee). In addition, it is always a negative factor in the evolution of osteoarthritis affecting joints of support or that bear weight, as it is the case of the lumbar spine, hips or feet.
Obesity is a major risk factor for developing osteoarthritis.
The age
Of course age is important, since the number of people affected by osteoarthritis increases gradually with age. The age is associated with aging of tissues and, therefore, also of the cartilage. In addition, with the age decreases the ability to repair and regeneration of cartilage from injuries.The inheritance
There are certain genetic factors that influence the development of osteoarthritis. In this way, has been that there are some families whose members are more likely to suffer from osteoarthritis. There are certain types of arthritis that have an important genetic component and that, somehow, could be considered as "hereditary" osteoarthritis. This is so in the case of arthritis of the joints of the fingers of the hands, which usually occurs in women of the same family, are usually transmitted from mothers daughters.The "mechanical" lesions
Some professions involve the realization of a repetition of movements and, therefore, the repetitive use of certain joints (workers, farmers, athletes, carpenters...). These efforts represent a sustained overload of certain joints for long periods. This conditions one injury to articulate that it favors the development of early osteoarthritis.Other factors that negatively affect the development of osteoarthritic processes are: repeated injuries, the lack of adequate physical activity (essential for the maintenance of an appropriate and a proper physical state of locomotor muscle tone), and the adoption of incorrect postures, as well as carrying out inappropriately on certain activities of daily living.
Bone density
Has been that you people have less bone mass; i.e., that they have more fragile bones, they have less risk of developing osteoarthritis. Therefore, osteoporosis (bone disease characterized by low bone mass, due to a softening of the bones) "protects" in some form of the risk of developing osteoarthritis.However, osteoporosis is a serious bone disease that can cause fractures of the bones, so it is essential to prevent it through exercise and an adequate intake of calcium (mainly present in dairy products).
WHAT SYMPTOMS CAUSES OSTEOARTHRITIS?
Osteoarthritis is a chronic disease, which develops very slowly. Its symptoms are unimportant in the beginning, progressing gradually with the passage of time.The fundamental complaint of patients with osteoarthritis is pain in the joint. Initially, the pain is discreet and only occurs when you will force the joint with important physical activity, giving spontaneously with the rest. Subsequently, if the disease progresses, the pain appears more easily and becomes more continuous. Less physical effort is required for the patient note discomfort.
Joint pain in osteoarthritis is greater at the beginning of the movement (when you start walking or incorporated in a Chair, for example). It is accompanied by a feeling of stiffness or numbness of the joint, which makes it difficult to move it freely. This pain and stiffness improved in a few minutes once the joint "heats up" with the exercise.
Sometimes, in the evolution of osteoarthritis episodes of decompensation of the symptoms occur. In these periods, which are of variable duration, the patient experiences a much more acute and intense pain that prevents you from moving the diseased joint. In addition, the pain is more continuous and unrelieved so easily with the rest. These offsets are often accompanied by the existence of an inflammation joint (synovial fluid spills) or tendinitis (inflammation of the tendons around the joint with osteoarthritis).
When osteoarthritis is not controlled and will reach more advanced stages of the disease, in addition to the pain, the patient complains of a limitation or reduction in movements that can be done with the joint (e.g., not can Flex the hip or the knee completely). Certain joints with osteoarthritis deformities and abnormalities in the alignment of the bones may also be seen.
Deformities in the lower limbs that appear in osteoarthritis of the knee.
It is important to note that there are a number of single, dependent on the personality of the patient, factors that influence even more than the severity of osteoarthritis in determining the symptoms that the patient is complaining. The perception of pain is influenced by circumstances emotional anxiety, stress, depressed mood and own individual sensitivity to pain.
In this way, people more sensitive to pain and patients with depressive or anxious personality complain much more severe symptoms. In addition, they experience a feeling of far greater disability that emotionally stable patients, even when the importance and severity of their injuries joint is minimal.
HOW IT IS DIAGNOSED OSTEOARTHRITIS?
The diagnosis of osteoarthritis is simple, and is based on the evaluation of symptoms and physical examination the doctor performing the patient. The doctor assesses what symptoms the patient has, where they are located, what pain, what circumstances make worse (to go up or down stairs, opening or closing valves...) or better (with the rest). Also interrroga on which other diseases suffers from the sick, what treatments you are receiving, and if he or a family member suffer or have suffered from some kind of rheumatic disease, trauma or injury joint before.With the physical examination, the doctor may see what are the affected joints and what degree of severity has osteoarthritis. To do so, the joint is inspected and is touching its surface to determine the trigger points. Also evaluates what range of mobility have, determining what are the movements that trigger symptoms.
X-rays can confirm the diagnosis of osteoarthritis, to be able to see typical radiologic changes of osteoarthritic processes in joints. The severity of osteoarthritis can be determined much more precisely by radiological studies.
Blood tests are of no use to diagnose osteoarthritis. All results that are determined are always normal in osteoarthritis, including so-called "tests" rheumatic. The only indication for them is to confirm with your normal diagnosis of osteoarthritis, discarding other rheumatic diseases that do produce some alterations in the laboratory tests. For example, the arthritis are altered the blood sedimentation rate, rheumatoid factor and other rheumatic tests; in gout, uric acid is high...
Other more modern and sophisticated tests (MRI, scan, bone scan) are not necessary for the study of a patient with osteoarthritis. The physician only consider indicated their realization in isolated cases in which suspected that, in addition to arthrosis, there is any other associated complications (break of meniscus in the knee, herniated disc or involvement of the spinal nerves in the osteoarthritis of spine, for example).
AS IT IS ARTHROSIS?
There is currently no treatment able to cure arthritis. However, we have, today, an important array of therapeutic measures to combat it. These measures include both drugs, physiotherapy treatments and rehabilitation, as ultimately of surgical interventions. By they prevent or reduce the symptoms of osteoarthritis, slow its progression, and ultimately improve the quality of life of patients with osteoarthritis.Osteoarthritis is not a serious illness, in the sense that neither kills nor shortens the life expectancy of patients. It remains a chronic disease, but today has been very significantly reduced the invalidity that had been implied in the past.
Patients achieve a significant relief of symptoms with the treatments, and can usually lead an almost normal life. To do this, and as in other diseases, early diagnosis is very important. The patient must be put in the hands of medical professionals and comply with all the recommendations and indications for the treatment. The doctor will order at every moment of the evolution when you should take medicines, and when and what kind of rehabilitation must be done.
The treatment of osteoarthritis consists of the combination of different measures. All of these are fundamental and complementary to achieve an adequate therapeutic response. They are as follows:
1. General rules
There are a whole series of recommendations for the osteoarthritic patients which aim to protect the joints of the extremities and spine. These tips are intended to slow the evolution of osteoarthritis, avoiding factors that damage the joints and favour the progression of the disease. They are as follows:- Balanced diet, including a diet for weight loss in patients with obesity. It is essential to correct the overweight to prevent osteoarthritis. In patients who already have arthritis, weight loss is associated with a better prognosis of the disease.
- Proper night's rest, including rest periods during the day. However, we must prevent the immobility total or during prolonged periods, which are harmful in the long run.
- The patient with osteoarthritis must adapt their activities and exercise that performed just physical ability. You must accept its limitations and understand that it can not play certain activities with the same ease as a person who is not suffering from osteoarthritis.
- Avoid movements causing pain in the joint, ensuring as far as possible alternatives for the realization of activities aroused by pain.
- Avoid positions and harmful activities, such as squatting, knees or stand for long time, walking carrying excessive weight or uneven terrain, up and down stairs...
- The use of a cane or crutch, which helps to download the body of the joint weight can be very effective in osteoarthritis of the hip or knee. Cane must be carried in the hand opposite to the most affected joint (for example, in the right knee osteoarthritis, cane must be in the left hand).
- In osteoarthritis of the hands, the use of tools and household utensils appropriate is recommended. They must be wide handle and low weight. For not forcing the joints use AIDS, such as electrical brelatas, for example.
- In osteoarthritis of the foot, the doctor may indicate the use of Orthopedic insoles that discharge painful joints, in some cases decreasing discomfort that occurs when walking.
2. physical exercise
Physical exercise is fundamental in the sick artrosico to maintain the mobility of joints and strengthen the muscles. It is essential to prevent the muscles to atrophy, since the evolution of osteoarthritis makes it worse.Each patient must adapt the kind of exercise physique made to their particular circumstances, as directed by your doctor. The exercise to be carried out is depending on the affected joint, arthrosis, age of the patient and prior training.
It is important that physical activity is done in a slow, progressive, gradually, without causing pain. It must be carried out on a regular basis and constant (ideally practice it every day), so that the exercise be incorporated into the daily routine of the patient.
In general, practiced in the style of "backs", swimming is an excellent exercise for osteoarthritis. The tours are also very desirable, although they must be adapted to the physical capacity in patients with osteoarthritis of the hip and knee. The bike can be an alternative to physical exercise in certain patients.
In addition, there are a series of rehabilitation exercises, designed specifically for each localization of osteoarthritis, which usually provide in the form of "tables of exercises". They are usually easy realization, although it agrees to carry out a correct learning with the help of a physical therapist. The doctor is who must instruct each patient kind of exercises, when and how often should be rehabilitation exercises for patients with osteoarthritis.
3. application of electrotherapy, heat and cold
The local application of cold is indicated only when there is a phase of acute inflammation in the artriculacion. This is done with a bag of ice wrapped in a cloth. Bags of frozen food (frozen, e.g. peas) are also useful.In the rest of the cases, it is usually more beneficial application of heat, which relieves the pain, stiffness, joint and muscle contractures of osteoarthritis. The application of heat can be done using a shower or hot bath or with a blanket or hair dryer. Hot paraffin baths are used for hands. The application of distributed heat is better in several times a day, in periods of 10 to 15 minutes.
Another form of treatment consists of applying different techniques of electrotherapy and rehabilitation, known commonly as "current". These techniques (short wave, ultrasound, magnetic therapy, laser), are given periodically in several sessions of treatment in rehabilitation centres.
4 medication
The drugs are useful in osteoarthritis to relieve pain, decrease inflammation joint when it exists and, ultimately, to improve the patient's symptoms. The doctor prescribes them at certain times of decompensation of osteoarthritis; However, in some patients taking may be needed indefinitely.The most commonly used drugs are (commonly known as "soothing") painkillers and anti-inflammatory drugs, which provide good control of symptoms. There are also other drugs, whose function is the modify the evolution of osteoarthritis, delaying its progression and also to improve the symptoms.
In addition, in certain moments, may be indicated the so-called infiltration. Infiltration is a technique which, by means of an injection into the joint or in the tissues that surround it, are introduced drugs to reduce inflammation and improve symptoms.
It is essential to take into account that all the medication always must be prescribed and controlled by a physician. Self-medication, should be avoided because it can have negative consequences in the form of adverse side effects.
5. surgical operations
When all the above measures have failed and the patient has advanced arthritis, that does not improve with treatments above exposed, the surgery is indicated. There are a series of interventions that allow, or else to correct injuries and deformities joint, either replace the damaged by a prosthetic joint. With surgery improves symptoms, especially pain, and mobility is preserved articulate. Orthopaedic Surgeons (trauma) are the specialists responsible for carrying out these operations.AS IT IS ARTHROSIS?
There is currently no treatment able to cure arthritis. However, we have, today, an important array of therapeutic measures to combat it. These measures include both drugs, physiotherapy treatments and rehabilitation, as ultimately of surgical interventions. By they prevent or reduce the symptoms of osteoarthritis, slow its progression, and ultimately improve the quality of life of patients with osteoarthritis.Osteoarthritis is not a serious illness, in the sense that neither kills nor shortens the life expectancy of patients. It remains a chronic disease, but today has been very significantly reduced the invalidity that had been implied in the past.
Patients achieve a significant relief of symptoms with the treatments, and can usually lead an almost normal life. To do this, and as in other diseases, early diagnosis is very important. The patient must be put in the hands of medical professionals and comply with all the recommendations and indications for the treatment. The doctor will order at every moment of the evolution when you should take medicines, and when and what kind of rehabilitation must be done.
The treatment of osteoarthritis consists of the combination of different measures. All of these are fundamental and complementary to achieve an adequate therapeutic response. They are as follows:
1. General rules
There are a whole series of recommendations for the osteoarthritic patients which aim to protect the joints of the extremities and spine. These tips are intended to slow the evolution of osteoarthritis, avoiding factors that damage the joints and favour the progression of the disease. They are as follows:- Balanced diet, including a diet for weight loss in patients with obesity. It is essential to correct the overweight to prevent osteoarthritis. In patients who already have arthritis, weight loss is associated with a better prognosis of the disease.
- Proper night's rest, including rest periods during the day. However, we must prevent the immobility total or during prolonged periods, which are harmful in the long run.
- The patient with osteoarthritis must adapt their activities and exercise that performed just physical ability. You must accept its limitations and understand that it can not play certain activities with the same ease as a person who is not suffering from osteoarthritis.
- Avoid movements causing pain in the joint, ensuring as far as possible alternatives for the realization of activities aroused by pain.
- Avoid positions and harmful activities, such as squatting, knees or stand for long time, walking carrying excessive weight or uneven terrain, up and down stairs...
- The use of a cane or crutch, which helps to download the body of the joint weight can be very effective in osteoarthritis of the hip or knee. Cane must be carried in the hand opposite to the most affected joint (for example, in the right knee osteoarthritis, cane must be in the left hand).
- In osteoarthritis of the hands, the use of tools and household utensils appropriate is recommended. They must be wide handle and low weight. For not forcing the joints use AIDS, such as electrical brelatas, for example.
- In osteoarthritis of the foot, the doctor may indicate the use of Orthopedic insoles that discharge painful joints, in some cases decreasing discomfort that occurs when walking.
- Postural recommendations to protect joint.
2. physical exercise
Physical exercise is fundamental in the sick artrosico to maintain the mobility of joints and strengthen the muscles. It is essential to prevent the muscles to atrophy, since the evolution of osteoarthritis makes it worse.Each patient must adapt the kind of exercise physique made to their particular circumstances, as directed by your doctor. The exercise to be carried out is depending on the affected joint, arthrosis, age of the patient and prior training.
It is important that physical activity is done in a slow, progressive, gradually, without causing pain. It must be carried out on a regular basis and constant (ideally practice it every day), so that the exercise be incorporated into the daily routine of the patient.
In general, practiced in the style of "backs", swimming is an excellent exercise for osteoarthritis. The tours are also very desirable, although they must be adapted to the physical capacity in patients with osteoarthritis of the hip and knee. The bike can be an alternative to physical exercise in certain patients.
In addition, there are a series of rehabilitation exercises, designed specifically for each localization of osteoarthritis, which usually provide in the form of "tables of exercises". They are usually easy realization, although it agrees to carry out a correct learning with the help of a physical therapist. The doctor is who must instruct each patient kind of exercises, when and how often should be rehabilitation exercises for patients with osteoarthritis.
3. application of electrotherapy, heat and cold
The local application of cold is indicated only when there is a phase of acute inflammation in the artriculacion. This is done with a bag of ice wrapped in a cloth. Bags of frozen food (frozen, e.g. peas) are also useful.In the rest of the cases, it is usually more beneficial application of heat, which relieves the pain, stiffness, joint and muscle contractures of osteoarthritis. The application of heat can be done using a shower or hot bath or with a blanket or hair dryer. Hot paraffin baths are used for hands. The application of distributed heat is better in several times a day, in periods of 10 to 15 minutes.
Another form of treatment consists of applying different techniques of electrotherapy and rehabilitation, known commonly as "current". These techniques (short wave, ultrasound, magnetic therapy, laser), are given periodically in several sessions of treatment in rehabilitation centres.
4 medication
The drugs are useful in osteoarthritis to relieve pain, decrease inflammation joint when it exists and, ultimately, to improve the patient's symptoms. The doctor prescribes them at certain times of decompensation of osteoarthritis; However, in some patients taking may be needed indefinitely.The most commonly used drugs are (commonly known as "soothing") painkillers and anti-inflammatory drugs, which provide good control of symptoms. There are also other drugs, whose function is the modify the evolution of osteoarthritis, delaying its progression and also to improve the symptoms.
In addition, in certain moments, may be indicated the so-called infiltration. Infiltration is a technique which, by means of an injection into the joint or in the tissues that surround it, are introduced drugs to reduce inflammation and improve symptoms.
It is essential to take into account that all the medication always must be prescribed and controlled by a physician. Self-medication, should be avoided because it can have negative consequences in the form of adverse side effects.
5. surgical operations
When all the above measures have failed and the patient has advanced arthritis, that does not improve with treatments above exposed, the surgery is indicated. There are a series of interventions that allow, or else to correct injuries and deformities joint, either replace the damaged by a prosthetic joint. With surgery improves symptoms, especially pain, and mobility is preserved articulate. Orthopaedic Surgeons (trauma) are the specialists responsible for carrying out these operations.TIPS ON ARTHRITIS
ARTHROSIS: What is osteoarthritis?

INITIAL SYMPTOMS
· Mechanical pain that appears with the movement and yields during the Sabbath.
· Difficulty performing everyday movements.
· Cracking noises, and crepitation when moving joints.
PROGRESSIVE SYMPTOMS
· Deep pain.
· Swelling and deformation of joints.
· Loss of mobility.
· Stiffness when you get up in the morning.



· It is a common condition, usually age-related.
· It mainly affects joints such as the knee, hip and shoulder.
· The joints become deformed by limiting the mobility of the patient
· The disease evolves over years becoming a chronic degenerative disease.
OSTEOARTHRITIS: PRECAUTIONS


· Keep your weight within appropriate limits.
· Moderate exercise without loading the joints.
· Avoid movements that require effort.
· Purchase positions suited to sitting up or lying down.



· The exercise indicated by your doctor.
· Try to sit and stand up progressively and with help...
· Avoid carrying heavy objects.
· Wear comfortable shoes.